Airway management is one of the most critical aspects of patient care, particularly in emergency situations, during surgery, and in intensive care units. Intubation—the process of inserting an endotracheal tube into a patient’s airway to secure it—is a life-saving procedure. However, the success of intubation largely depends on the tools used to guide the insertion of the tube, with the intubation stylet being one of the most essential devices in this process. In recent years, the single-use intubation stylet has gained significant attention in healthcare settings due to its reliability, sterility, and efficiency.
This article explores how the use of single-use intubation stylet can improve patient outcomes, enhance safety, and streamline the intubation process.
1. Enhanced Sterility Reduces the Risk of Infection:
One of the most significant advantages of using single-use intubation stylets is the assurance of sterility. Intubation is an invasive procedure that involves inserting a tube into a patient’s trachea. If not performed with sterile equipment, there is a risk of introducing pathogens into the airway, which can lead to serious infections, including ventilator-associated pneumonia (VAP) or sepsis.
Reusable intubation stylets, while effective, often require meticulous cleaning and sterilization. Even with proper protocols in place, the possibility of residual contaminants or inadequate sterilization remains, especially when time and resources are limited in emergency care settings.
Single-use intubation stylets, however, are pre-sterilized and disposable, eliminating the risk of cross-contamination. By using a fresh, sterile stylet for each intubation, healthcare providers significantly reduce the chances of introducing infections to the patient. This heightened level of infection control directly contributes to improved patient outcomes, particularly for those who may already be vulnerable due to underlying conditions or recent surgery.
2. Faster Intubation Process Improves Patient Safety:
In emergency medical settings, rapid airway management is essential to prevent hypoxia (lack of oxygen) and ensure patient survival. In cases of trauma, cardiac arrest, or respiratory failure, securing the airway quickly can make the difference between life and death. Intubation in these critical situations requires speed and precision, which is where single-use intubation stylets can make a significant impact.
Unlike reusable stylets that require time for cleaning, inspection, and sterilization, single-use intubation stylets come pre-packaged and ready for immediate use. This minimizes the time spent preparing the equipment, allowing healthcare providers to focus entirely on securing the patient’s airway. The convenience of having a sterile, disposable stylet ready to use in emergencies means that intubation can be performed more quickly, reducing the risk of complications such as aspiration, hypoxia, or respiratory distress.
Additionally, the straightforward design of many single-use intubation stylets allows for easier handling, making it simpler for healthcare providers to manipulate the tube and secure the airway in high-pressure situations. This ease of use contributes to faster, more effective intubations, further improving patient outcomes.
3. Reduced Risk of Equipment Failure and Malfunction:
Reusable medical equipment, including intubation stylets, can degrade over time. Frequent use, repeated sterilization, and wear and tear can compromise the integrity and function of reusable stylets, increasing the risk of malfunction during critical procedures. A malfunctioning or damaged stylet can hinder the intubation process, potentially causing delays, difficulty in securing the airway, and increased risk to the patient.
Single-use intubation stylets, on the other hand, are disposed of after each use, ensuring that they are always in optimal condition for every intubation procedure. Each stylet is manufactured to meet strict quality control standards and is guaranteed to be free from defects. As a result, healthcare providers can rely on the single-use stylet to perform its intended function without the risk of malfunction or failure. This reliability is crucial, particularly during emergency intubations where there is little room for error.
The assurance that the equipment will function properly every time contributes to a smoother intubation process, improving the likelihood of a successful outcome and reducing complications during airway management.
4. Improved Patient Comfort and Reduced Trauma:
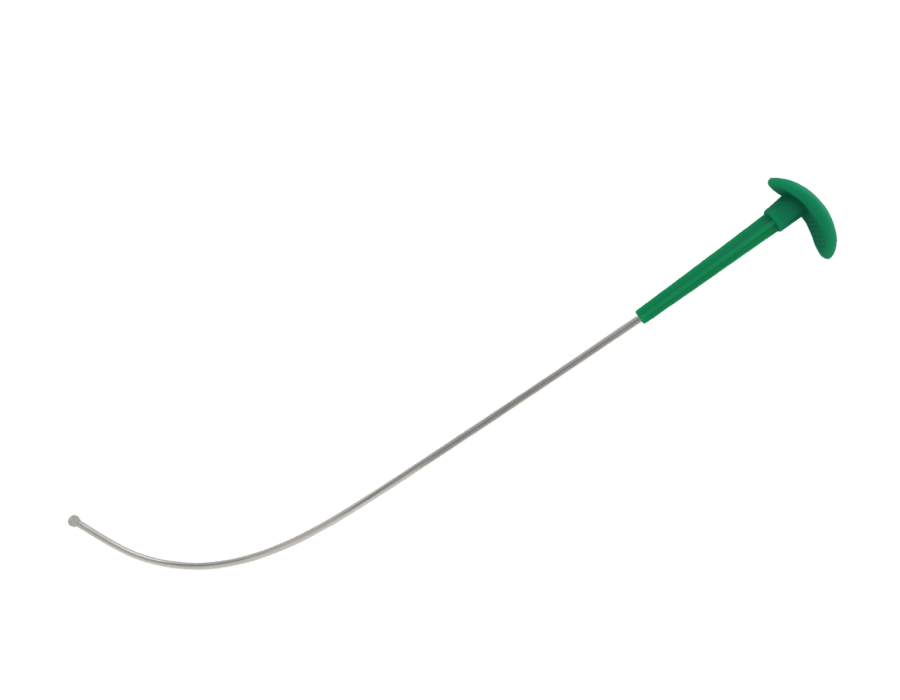
In difficult intubations, where the airway is challenging to access or the patient has an abnormal anatomy, the choice of intubation stylet can significantly affect the outcome. A flexible and well-designed stylet allows healthcare providers to maneuver the endotracheal tube more easily, minimizing the amount of force required to navigate the patient’s airway. This is particularly important for reducing patient discomfort and preventing damage to delicate tissues in the airway.
Single-use intubation stylets are often designed with flexibility in mind, allowing healthcare providers to better adapt to a patient’s specific anatomical needs. Some models also offer adjustable curvatures, which can be customized to ensure optimal tube placement. The more effective the stylet in guiding the tube with precision, the less force is needed to complete the intubation, reducing trauma to the patient’s throat, larynx, and trachea.
Minimizing trauma not only improves patient comfort but also reduces the risk of complications such as post-intubation sore throat, hoarseness, or airway injury. By using a stylet that enhances the overall intubation experience, patients benefit from a smoother, more comfortable procedure, leading to better long-term outcomes.
5. Minimization of Cross-Contamination and Hospital-Acquired Infections:
Cross-contamination is a constant concern in healthcare settings, especially when medical equipment is reused. Even with the best cleaning protocols in place, reusable equipment can sometimes fail to meet sterility standards, putting both patients and healthcare workers at risk for hospital-acquired infections (HAIs). Intubation stylets, which are used in highly invasive procedures, are particularly vulnerable to contamination.
The single-use nature of these stylets removes the possibility of cross-contamination between patients, significantly reducing the risk of HAIs. In busy hospitals or intensive care units where multiple patients are treated each day, the ability to use a fresh stylet for every intubation ensures that the procedure is performed with the highest level of infection control. This reduction in cross-contamination helps prevent the spread of infections such as ventilator-associated pneumonia, urinary tract infections, or bloodstream infections, all of which can lead to longer hospital stays, additional treatments, and increased mortality rates.
By mitigating the risk of HAIs, single-use intubation stylets play a critical role in improving patient safety and overall healthcare outcomes.
6. Cost-Effectiveness through Reduced Complications:
Although single-use intubation stylets may have a higher upfront cost compared to reusable options, they can ultimately prove to be more cost-effective in the long term. Reusable stylets require regular cleaning, sterilization, and occasional repair or replacement. These ongoing costs, along with the labor involved in maintaining reusable equipment, can add up over time.
Moreover, the risk of complications from infection or equipment failure associated with reusable devices can lead to increased healthcare costs, including longer hospital stays, additional treatments, and potential litigation in cases of medical malpractice. By reducing the risk of infection and malfunction, single-use stylets help minimize these costs and reduce the overall financial burden on healthcare institutions.
In the long run, the use of single-use intubation stylets can contribute to better resource allocation, allowing healthcare facilities to invest in high-quality, disposable equipment that improves patient outcomes while reducing the need for costly interventions.
Conclusion:
The single-use intubation stylet is a game-changer in airway management, offering a range of benefits that directly contribute to improved patient outcomes. By ensuring sterility, improving the speed and efficiency of intubations, reducing the risk of equipment failure, and minimizing complications, single-use stylets enhance patient safety and comfort. Moreover, by preventing cross-contamination and hospital-acquired infections, they play a crucial role in maintaining the health and well-being of both patients and healthcare providers.
In high-stakes environments like emergency care, anesthesia, and intensive care, the choice to use a single-use intubation stylet can make all the difference in ensuring successful, complication-free intubations. By investing in these disposable tools, healthcare providers can offer better care, reduce risk, and ultimately improve the overall outcomes for their patients.




Comments