If you’re a healthcare provider or run a small DME business in the USA, you already know one thing—billing for DME supplies can feel like solving a Rubik’s cube blindfolded. Between payer rules, documentation hassles, modifiers, and ever-changing policies, it’s easy to get overwhelmed.
But here’s the good news: once you understand the core process and avoid a few common pitfalls, billing becomes surprisingly manageable.
In this guide, I’ll walk you through DME billing in a clear, relaxed, no-nonsense way that’s actually helpful.
What Exactly Counts as DME?
Durable Medical Equipment (DME) includes reusable medical devices that help patients at home.
A few common examples:
- Wheelchairs (manual or power)
- Walkers, canes, crutches
- CPAP/BiPAP machines
- Nebulizers
- Blood glucose monitors
- Orthotics and prosthetics
- Hospital beds and supplies
If it’s meant to last and supports the patient’s long-term condition, it’s probably DME.
Why DME Billing Feels So Complicated
Let’s be honest—billing for DME supplies in the USA is messy mostly because:
- Coverage rules vary across payers
- Every item has unique HCPCS codes
- Modifiers change reimbursement
- Documentation requirements are strict
- Prior authorization is often mandatory
In short, it’s not that you’re doing anything wrong… the system itself is just complex.
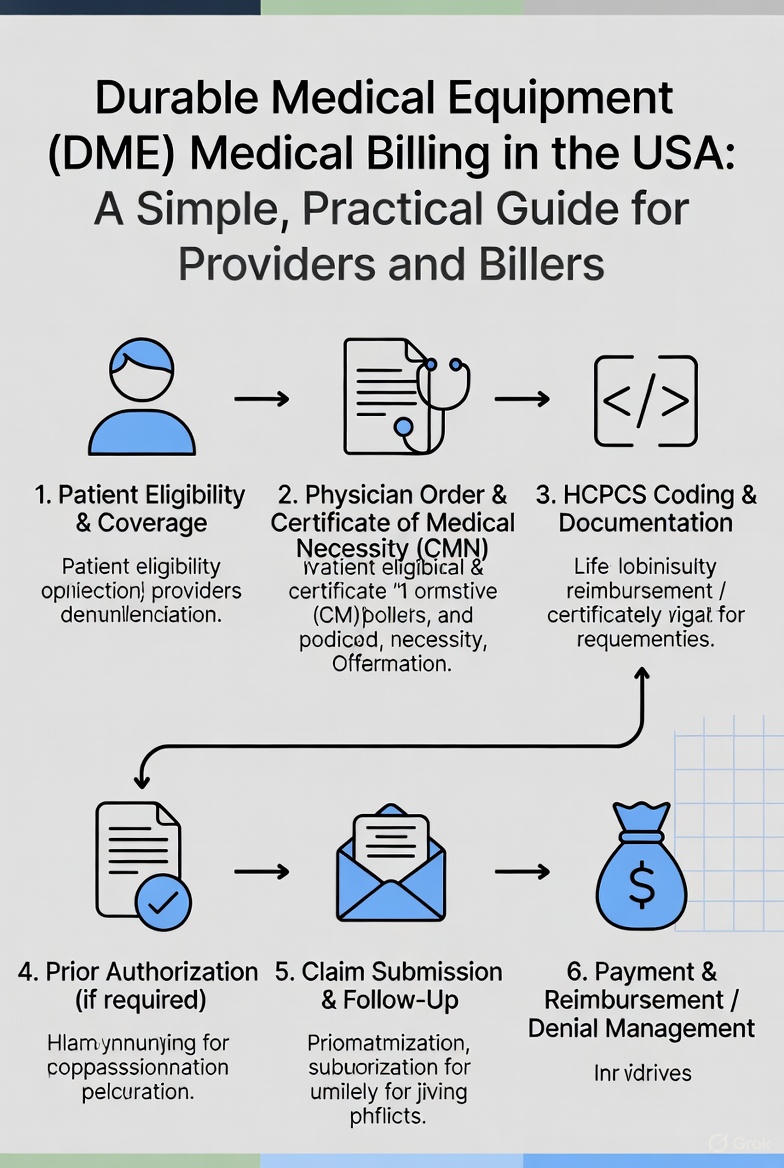
Step-by-Step Breakdown: Billing for DME Supplies
Here’s the easiest way to understand the workflow:
1. Verify Patient Insurance (Don’t Skip This!)
Before delivering equipment, always check:
- Eligibility
- DME coverage under the plan
- Copay/coinsurance
- Deductible status
- Prior authorization rules
This one step can save you days of denial headaches.
2. Gather All Required Documentation
Payers want proof — and lots of it.
Make sure you have:
- Detailed physician order
- Face-to-face encounter notes
- Certificate of Medical Necessity (CMN), if required
- Supporting test results
- Proper diagnosis (ICD-10-CM) codes
Rule of thumb: If it’s not documented, it didn’t happen.
3. Use the Correct HCPCS Codes + Modifiers
Each supply has a specific code.
For example:
- E0601 – CPAP machine
- A7030–A7039 – CPAP accessories
- E0143 – Walker
- A4253 – Blood glucose test strips
And don't forget modifiers like:
- NU – New equipment
- RR – Rental
- MS – Maintenance
- KX – Documentation on file
- GA/GY/GZ – Liability modifiers
One wrong modifier can tank the whole claim.
4. Submit the Claim Cleanly
Most DME providers use:
- CMS-1500 form
- EDI/837P for electronic submission
Double-check:
- NPI
- Taxonomy
- Place of service
- Units
- Pricing
Clean claims get paid faster — simple as that.
5. Track the Claim Until It Pays
Don’t just submit and forget.
Follow up with payers through:
- ERA/EOB
- Portal status checks
- Call-ins (if absolutely needed)
If you spot a denial, fix it quickly. DME denials pile up if not handled right away.
Common Mistakes That Slow Down DME Reimbursement
A lot of providers make the same avoidable errors. Keep an eye out for:
- Missing KX modifier
- Wrong HCPCS units
- Expired authorization
- Delivering equipment before approval
- Insufficient physician documentation
- Wrong diagnosis linkage
Avoid these, and you’ll immediately reduce your denial rate.
Tips to Make DME Billing Way Easier
Here’s the stuff seasoned billers swear by:
- Create checklists for every type of equipment
- Maintain templates for orders and medical necessity notes
- Train staff to catch mistakes before claims go out
- Stay updated with CMS and payer-specific rules
- Audit claims monthly to spot patterns early
- Keep communication tight with physicians (documentation is everything)
You’d be surprised how much smoother things get with even small improvements.
How Billing Companies Help (If You Want to Outsource)
If DME billing isn’t your strong suit — or it’s eating too much time — outsourcing can help you:
- Cut down denials
- Speed up payments
- Handle prior auths
- Stay compliant with CMS rules
- Reduce administrative stress
It’s not mandatory, but for many small DME suppliers, it’s a lifesaver......(Contact Us)
FAQs About Billing for DME Supplies
1. Does every DME item need prior authorization?
Nope. But a lot of high-cost or rental items do. Always check the payer portal before delivery.
2. Why are my claims getting denied for “lack of medical necessity”?
Usually because documentation didn’t clearly justify the patient’s need. Tighten the notes, add details, and attach supporting records.
3. How often should I bill for recurring supplies?
Most payers have set refill limits — like 30-day or 90-day cycles. Billing too early or too late causes denials.
4. How long should I keep DME documentation?
Medicare recommends at least 7 years. Keep everything digital and organized.
5. Can patients upgrade equipment and pay the difference?
Sometimes, yes — but upgrades must be properly documented, and the patient must sign an ABN when Medicare is involved.




.png)
Comments