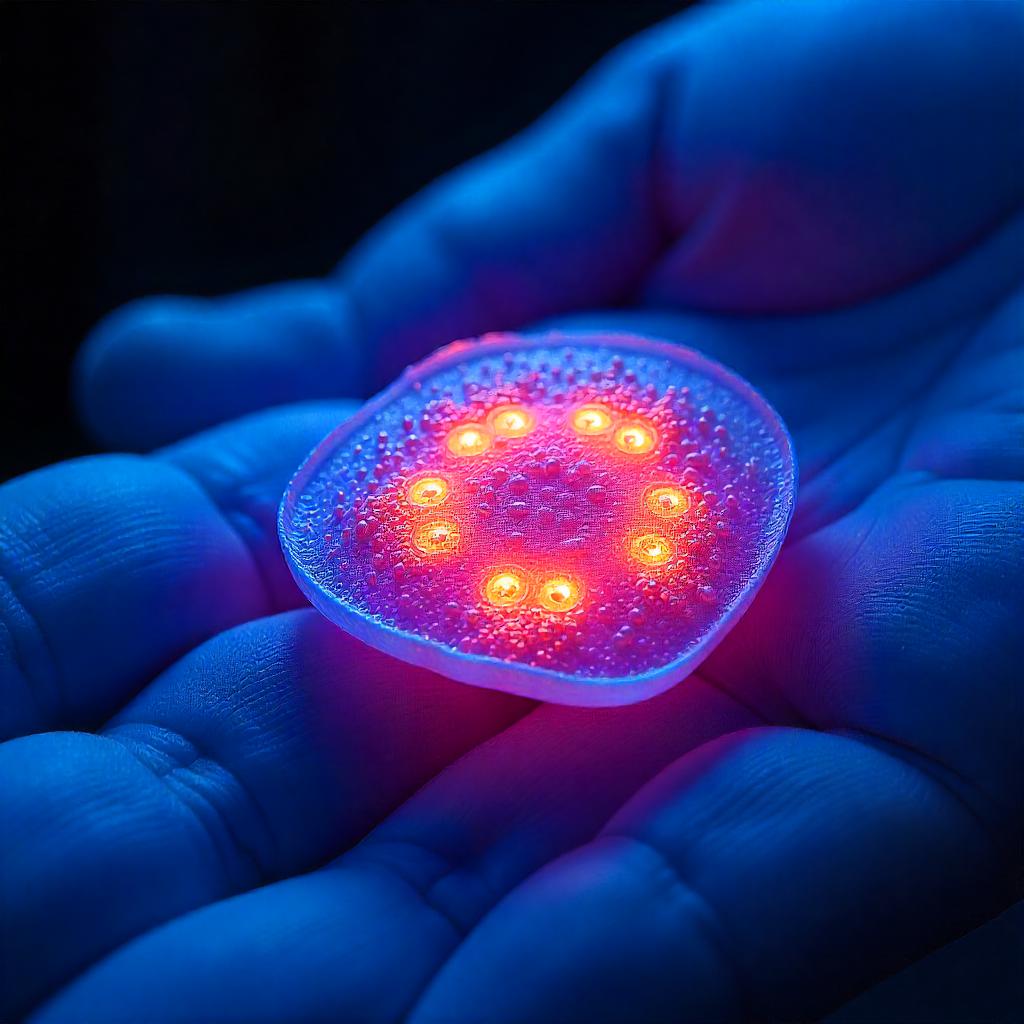
In recent years, regenerative medicine has transformed how clinicians approach wound healing and tissue repair. Among the most promising biologic materials used today is a specialized tissue derived from the innermost layer of the placenta—known in clinical applications as an allograft amniotic membrane. This natural tissue is recognized for its structural and bioactive properties, playing a pivotal role in supporting healing in a variety of medical settings.
The inner amniotic membrane, sourced ethically from donated human placental tissue following cesarean deliveries, contains essential components such as growth factors, collagen, cytokines, and extracellular matrix proteins. These elements collectively create an environment conducive to tissue regeneration, cellular migration, and angiogenesis, all of which are critical in the body’s natural healing processes. Additionally, the tissue has inherent anti-inflammatory, antimicrobial, and antifibrotic characteristics, making it highly suitable for managing both acute and chronic wounds.
One of the most important benefits of this biological material is its ability to act as a temporary barrier over wounds. By covering exposed tissue, it helps protect the wound bed from contamination while maintaining a moist environment, which is widely known to accelerate healing and reduce pain. This quality makes the membrane particularly valuable in the treatment of diabetic ulcers, venous leg ulcers, pressure sores, surgical incisions, and traumatic injuries.
Another advantage lies in its minimal immunogenicity. Unlike synthetic grafts or xenografts, this tissue is generally well tolerated by the human body, reducing the risk of immune response or rejection. Its application does not typically require extensive preparation, and the material conforms easily to irregular wound surfaces, enhancing both ease of use and patient comfort.
In surgical fields such as orthopedics, podiatry, plastic surgery, and ophthalmology, this regenerative tissue is being widely adopted for soft tissue repair and reconstruction. Surgeons utilize it not only to enhance healing but also to reduce postoperative complications such as scarring or infection. In eye care, for instance, the tissue is used to treat corneal defects and conjunctival reconstruction, with encouraging clinical outcomes.
From a practical standpoint, processed versions of this biologic material are available in dehydrated or lyophilized forms, allowing for ambient storage and extended shelf life. This convenience ensures that it can be readily accessed in outpatient clinics, operating rooms, or emergency settings without the need for complex logistics.
As research in tissue engineering progresses, the clinical value of placental-derived products continues to rise. Studies support their effectiveness in reducing healing times, improving patient outcomes, and offering a less invasive alternative to traditional grafting techniques. The integration of these materials into routine clinical practice reflects a broader shift toward biologically driven, patient-centered care.
Healthcare professionals looking to enhance their wound care strategies are increasingly turning to solutions that align with the body’s natural regenerative capacity. As this field evolves, products built on biologic principles will continue to play a crucial role in redefining the future of healing.




Comments