In today’s healthcare ecosystem, precision in billing isn’t just a matter of compliance—it’s the difference between steady cash flow and mounting denials. Every claim that leaves your practice reflects hours of work, yet a small coding or data error can trigger delays or outright rejections. This is where Claim Scrubbing Services come into play - acting as a critical safeguard that filters out mistakes before they reach the payer’s system. At Best Medical Billing, we’ve seen firsthand how advanced claim scrubbing transforms billing accuracy, reduces revenue leakage, and accelerates reimbursements.
Understanding the Role of Claim Scrubbing
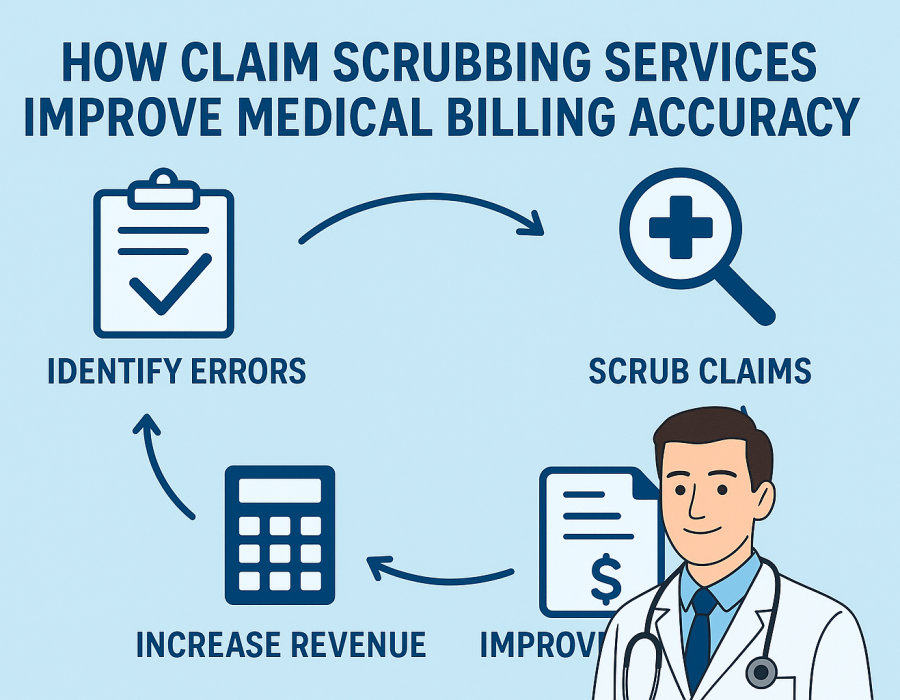
Claim scrubbing is the process of meticulously reviewing medical claims before submission to ensure every entry meets payer and regulatory requirements. Think of it as a quality control stage that identifies inconsistencies, missing modifiers, or incorrect CPT codes—issues that typically lead to denials. The aim is to clean the claim of any potential red flags so it passes the payer’s automated edits seamlessly.
In simple terms, scrubbing ensures that your claim doesn’t just go out fast—it goes out right the first time. For healthcare practices juggling patient care and administrative work, that accuracy is invaluable.
Why Accuracy in Billing Matters More Than Ever
Even minor errors can have major financial consequences. A mistyped patient ID, an outdated diagnosis code, or an invalid NPI number can push claims into the denial pile. Reworking those claims costs time and money, often eating into staff productivity and delaying payment cycles.
With Claim Scrubbing Services, every detail is checked against payer-specific rules, coding standards, and compliance frameworks such as ICD-10 and CPT. This proactive validation means your claims are much more likely to be accepted on the first submission—cutting rework time and improving overall cash flow.
Key Benefits of Claim Scrubbing Services
1. Higher First-Pass Resolution Rate
A robust scrubbing process identifies potential denials before submission. Practices that use dedicated Claim Scrubbing Services often see first-pass acceptance rates climb above 95%. That means fewer claims bounce back and more payments come in on time.
2. Reduced Administrative Workload
Without scrubbing, billing staff spend hours chasing errors, resubmitting claims, and managing payer feedback. Automated scrubbing eliminates repetitive tasks, allowing your team to focus on patient care and strategic revenue cycle improvements.
3. Enhanced Compliance and Coding Accuracy
Regulatory compliance is non-negotiable in healthcare billing. Claim scrubbers validate every code against the latest federal and payer-specific rules. This protects your organization from audits, penalties, and unnecessary denials.
4. Data-Driven Insights for Better Performance
Advanced scrubbing tools provide analytical feedback. At Best Medical Billing, we use this data to identify recurring errors, refine coding patterns, and guide staff training. This continuous improvement loop strengthens billing accuracy over time.
5. Accelerated Cash Flow
Clean claims lead to faster payment cycles. When claims are accurate, they get processed promptly, improving revenue predictability and overall financial health for your practice.
How Best Medical Billing Enhances Claim Scrubbing Efficiency
At Best Medical Billing, our claim scrubbing process combines technology, compliance expertise, and human oversight. We integrate AI-powered validation tools that cross-check each claim against payer databases and coding protocols, ensuring precision from start to finish.
Our specialists also manually review complex claims—especially those involving multiple modifiers, secondary insurances, or high-value procedures—to guarantee error-free submissions. This hybrid model ensures that every claim meets both the technical and contextual accuracy required by insurers.
We also tailor our Claim Scrubbing Services to the unique workflows of each client. Whether you’re a small private practice or a multi-specialty clinic, we customize rules, templates, and edit checks to match your specific payer mix and service types.
Common Errors Detected Through Claim Scrubbing
Claim scrubbing systems are designed to catch errors before they become denials. Here are some examples:
- Incorrect or missing patient demographics – A single wrong digit in a patient ID or date of birth can lead to rejection.
- Incompatible CPT and ICD-10 codes – Mismatched codes between procedure and diagnosis.
- Invalid or missing modifiers – Common in multi-procedure claims.
- Provider credential issues – Incorrect or expired NPI numbers.
- Billing for non-covered services – Avoids wasted efforts on non-reimbursable procedures.
Each of these errors, if unchecked, can slow down reimbursements and damage a provider’s cash flow.
Why Partnering with Experts Like Best Medical Billing Makes a Difference
Many practices still rely on in-house staff or outdated systems that can’t keep up with constant payer and coding updates. Best Medical Billing stays ahead of these changes, ensuring every claim aligns with the latest CMS and commercial payer requirements.
Our team also provides detailed claim feedback reports so providers understand where issues arise and how to prevent them in the future. The result? Long-term efficiency and measurable growth in billing performance.
Final Thoughts
Accuracy in medical billing isn’t a luxury - it’s a necessity for financial stability and compliance. Claim Scrubbing Services act as the first line of defense against denials, helping healthcare providers maintain clean, compliant, and timely claim submissions.
At Best Medical Billing, our goal is to make that accuracy effortless. Through advanced technology, expert coders, and continuous process optimization, we help practices minimize errors, speed up payments, and build a stronger revenue cycle foundation.




Comments